Beginning with Global health policies after COVID-19, the narrative unfolds in a compelling and distinctive manner, drawing readers into a story that promises to be both engaging and uniquely memorable.
As the world navigates the aftermath of the COVID-19 pandemic, the focus shifts towards reevaluating and reshaping global health policies to adapt to the new normal.
Global Health Policies Overview

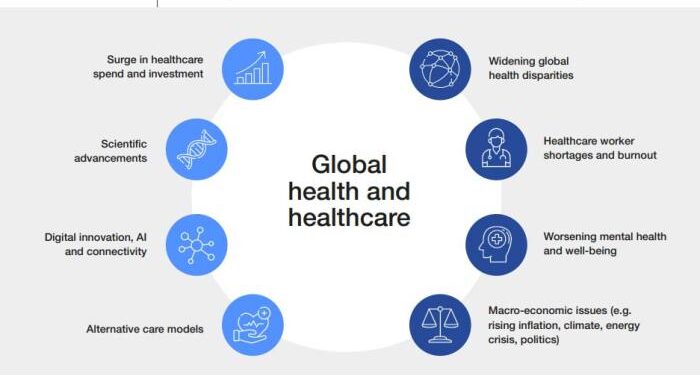
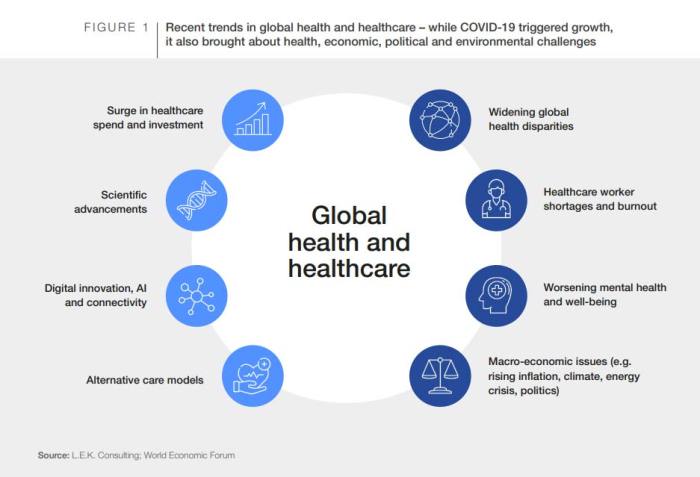
The COVID-19 pandemic has significantly impacted global health policies, prompting a reevaluation and adaptation of existing strategies to better respond to public health crises. Pre-COVID-19 health policies focused on routine healthcare services, with limited preparedness for a pandemic of this scale.
Post-COVID-19, there is a greater emphasis on pandemic preparedness, rapid response mechanisms, and international collaboration to mitigate the spread of infectious diseases.
Impact of COVID-19 on Global Health Policies
The emergence of COVID-19 exposed gaps in global health policies, highlighting the need for a more coordinated and proactive approach to public health. Countries worldwide have revised their health policies to include measures such as lockdowns, mass testing, contact tracing, and vaccination campaigns to contain the virus.
The pandemic has underscored the importance of investing in healthcare infrastructure, strengthening healthcare systems, and prioritizing public health initiatives.
Comparison of Pre-COVID-19 and Post-COVID-19 Health Policies
Pre-COVID-19 health policies were primarily focused on delivering routine healthcare services and addressing non-communicable diseases. In contrast, post-COVID-19 adaptations have shifted towards enhancing pandemic preparedness, improving surveillance systems, and ensuring access to essential healthcare services during emergencies. The pandemic has accelerated the adoption of digital health technologies, telemedicine, and remote monitoring to facilitate healthcare delivery while minimizing physical contact.
Key Stakeholders Shaping Global Health Policies Post-Pandemic
Key stakeholders involved in shaping global health policies post-pandemic include governments, international organizations (such as the World Health Organization), non-governmental organizations, healthcare providers, pharmaceutical companies, and research institutions. These stakeholders collaborate to develop strategies for vaccine distribution, healthcare workforce training, public health campaigns, and policy implementation to address current and future health threats on a global scale.
Public Health Infrastructure
The foundation of a strong global health policy lies in robust public health infrastructure that can effectively respond to health crises and protect populations worldwide. Investments in healthcare systems play a crucial role in ensuring countries are better equipped to handle future health emergencies.
By allocating resources towards improving healthcare facilities, training healthcare workers, and enhancing disease surveillance systems, countries can enhance their preparedness for any potential health threats.
Successful Public Health Initiatives
- Mass vaccination campaigns: Countries that have successfully implemented large-scale vaccination programs have significantly reduced the burden of preventable diseases and improved overall public health outcomes. For example, the Global Polio Eradication Initiative has made remarkable progress in eradicating polio through coordinated vaccination efforts.
- Health education and promotion: Public health initiatives that focus on educating communities about preventive measures, healthy behaviors, and disease transmission have been effective in reducing the spread of infectious diseases. Programs like the Clean Hands Save Lives campaign have raised awareness about the importance of hand hygiene in preventing infections.
- Healthcare workforce training: Investing in training programs for healthcare workers, including doctors, nurses, and community health workers, can strengthen the healthcare system's capacity to respond to emergencies. Countries like Rwanda have successfully implemented training programs to increase the number of skilled healthcare professionals in underserved areas.
International Collaboration
International collaboration plays a crucial role in shaping global health policies after the COVID-19 pandemic. By working together, countries can effectively address cross-border health challenges, share resources, and exchange information on a global scale.
Effective Cross-Border Health Challenges Address
- Establishing early warning systems for potential health threats that can quickly spread across borders.
- Coordinating efforts to contain infectious diseases and prevent their spread to neighboring countries.
- Developing joint response mechanisms to handle health emergencies that require international assistance.
Challenges and Benefits of Sharing Resources and Information
- Challenges:
- Ensuring equitable distribution of resources among countries with varying levels of economic development.
- Addressing concerns related to data privacy and security when sharing sensitive health information.
- Negotiating agreements on intellectual property rights for vaccines and treatments developed through international collaborations.
- Ensuring equitable distribution of resources among countries with varying levels of economic development
- Benefits:
- Rapid sharing of best practices and lessons learned from different countries' experiences in combating the pandemic.
- Pooling resources to accelerate research and development of vaccines, treatments, and diagnostics.
- Building trust and fostering goodwill among nations through joint efforts to improve global health outcomes.
Health Equity and Access
The COVID-19 pandemic has shed light on the existing disparities in health equity and access to healthcare services worldwide. Marginalized communities, including low-income populations, ethnic minorities, and rural areas, have been disproportionately affected by the pandemic, facing barriers in accessing testing, treatment, and vaccines.
Impact of COVID-19 on Health Equity
The pandemic has exacerbated inequalities in healthcare access, with marginalized communities facing higher rates of infection, severe illness, and mortality. Limited access to healthcare facilities, lack of health insurance, and systemic barriers have further widened the gap in health outcomes.
Strategies for Equitable Distribution
- Implement targeted outreach and education programs to ensure vulnerable populations are informed about available healthcare services and resources.
- Prioritize equitable distribution of vaccines and treatments to areas with higher infection rates and vulnerable populations.
- Strengthen healthcare infrastructure in underserved communities to improve access to quality care and services.
Addressing Disparities in Healthcare Access
- Develop policies that focus on addressing social determinants of health, such as poverty, education, and housing, to reduce disparities in healthcare access.
- Promote diversity and inclusion in healthcare leadership and workforce to better represent the populations they serve.
- Support community-based healthcare initiatives that aim to provide culturally sensitive care to diverse populations.
Ending Remarks
In conclusion, the discussion on global health policies after COVID-19 underscores the need for collaborative efforts, equity in healthcare access, and strengthened public health infrastructure to ensure a healthier and more resilient future for all.
FAQ Explained
How has COVID-19 impacted global health policies?
COVID-19 has highlighted the importance of robust public health systems and international collaboration in shaping global health policies for future pandemics.
What are some successful public health initiatives post-COVID-19 that can serve as models?
Initiatives such as vaccine distribution programs, telemedicine services, and community health outreach have shown promise in shaping post-pandemic health policies.
How can global health policies address disparities in healthcare access?
Global health policies can focus on equitable distribution of vaccines, treatments, and healthcare resources, along with addressing socio-economic factors that contribute to healthcare disparities.